
Considering the aforementioned study results, diabetes has become a major health issue due to its high related costs, both direct and indirect, for the health care systems. The effect(s) of the frequency of SMBG on glycemic control is controversial because although most studies show improvements in glycemic control with higher SMBG frequencies, in most of them the patients were still out of goal for good glycemic control. In general, there is a high degree of variability in the daily frequency of SMBG between patients, which range between one and five or more times daily. However, there is a considerable gap between the recommended and the reported frequencies of SMBG in T1D patients.
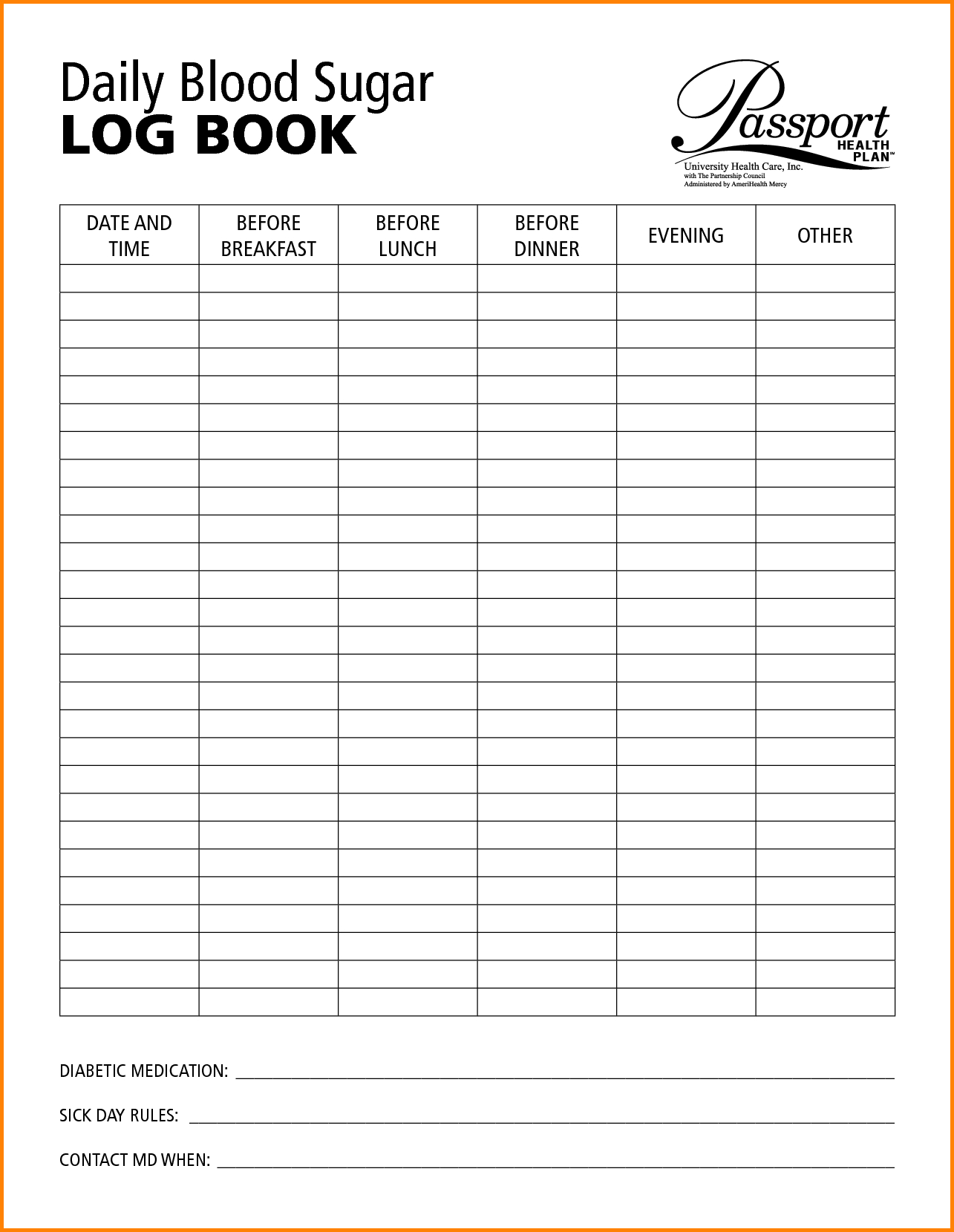
Currently, many guidelines for SMBG exist worldwide, such as those from ADA and the Brazilian Diabetes Society (SBD), which recommend at least three SMBG daily in patients with T1D. In developing countries, the cost of the strips and the compliance of the patients in bringing the glucometer to routine clinical visits, an important component for comparing data with the logbook, could also be significant barriers. Despite the aforementioned advantages, there are many barriers for the effective implementation of SMBG into routine clinical care that include poor education, fear of finger prick-related pain and difficulty in using the results to adjust insulin dosage. In this study, the majority of patients was under continuous subcutaneous insulin infusion (CSII) therapy and performed self-monitoring of blood glucose (SMBG) 4–6 times per day, which is currently an important tool for diabetes care that helps patients, caregivers and the diabetes team to adjust insulin therapy during hypoglycemia, hyperglycemia, physical activity, stress, illness and carbohydrate counting.
A recent multicenter study conducted in the United States of America (USA), the Type 1 Diabetes Exchange study, showed that the majority of T1D patients across all age-groups did not meet the American Diabetes Association’s (ADA) target for good glycemic control and showed an overall mean glycated hemoglobin (HbA1c) of 8.4% (68 mmol/mol). Nevertheless, in routine clinical practice, attaining adequate glycemic control remains a challenge mainly in developing countries and among minorities.
Diabetes logbook x trial#
Treatment includes intensive insulin therapy and non-pharmacological therapies, both important tools for obtaining an adequate glycemic control that is necessary to avoid or postpone diabetes-related chronic complications as has been demonstrated by the Diabetes Control and Complications Trial (DCCT) and the Epidemiology of Diabetes Interventions and Complications (EDIC) study. Type 1 diabetes (T1D) is a chronic disease with an incidence rate that is increasing worldwide. Adherence to diet was the main factor related to the agreement, but the supply of strips by SUS should also be considered in clinical practice. Our study revealed that the majority of T1D patients that were followed at a tertiary center did not have significant agreement between glycaemia obtained from a glucometer and a logbook. Significant difference was noted between baseline and final HbA1c, respectively. Multivariate analysis of this agreement (as a dependent variable) showed that adherence to diet was the only significant independent variable. Patients from group 1 presented a lower mean glycated hemoglobin (HbA1c) (p = 0.03) and a tendency to have a lower baseline HbA1c (p = 0.08), they received more frequently strips for glucose monitoring from the Sistema Único de Saúde (SUS) (p = 0.047) and were more adherent to the prescribed diet (p = 0.01) than patients from group 2. In 41 (26.8%) of the patients there was an agreement (group 1). Overall, for 112 (73.2%) of the patients, we found no agreement between glycaemia obtained from a glucometer and the logbook (group 2).

Resultsĭata were obtained from 158 patients. All consecutive patients with clinical diagnosis of T1D that attended the Diabetes Unit between April and June 2017 were enrolled in this study. This was a prospective observational cohort study conducted at the Diabetes Unit at Rio de Janeiro’s State University, between May 2017 and May 2018. The primary objective of this study was to evaluate the demographic, clinical, social-educational determinants and diabetes management factors that have influenced the agreement between glycaemia obtained from a glucometer and logbook the second objective was to evaluate the influence of the above-mentioned factors on glycemic control and its trajectories in Type 1 diabetes (T1D) over 1 year follow-up period during routine clinical practice.


 0 kommentar(er)
0 kommentar(er)
